International bi-monthly journal of cell signaling, tissue protection, and translational research.
Timing of angiography in out-of-hospital cardiac arrest patients with an initial shockable rhythm and without ST-segment elevation: a meta-analysis of randomized controlled trials
Bethany Alice Lane1,2, Heerajnarain Bulluck3,4
Author Affiliations


- 1Imperial College, London, UK.
- 2St. Bartholomew's Hospital, London, UK.
- 3Yorkshire Heart Centre, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust, Leeds, UK.
- 4Leeds Institute of Cardiovascular and Metabolic Medicine, University of Leeds, Leeds, UK.
Abstract
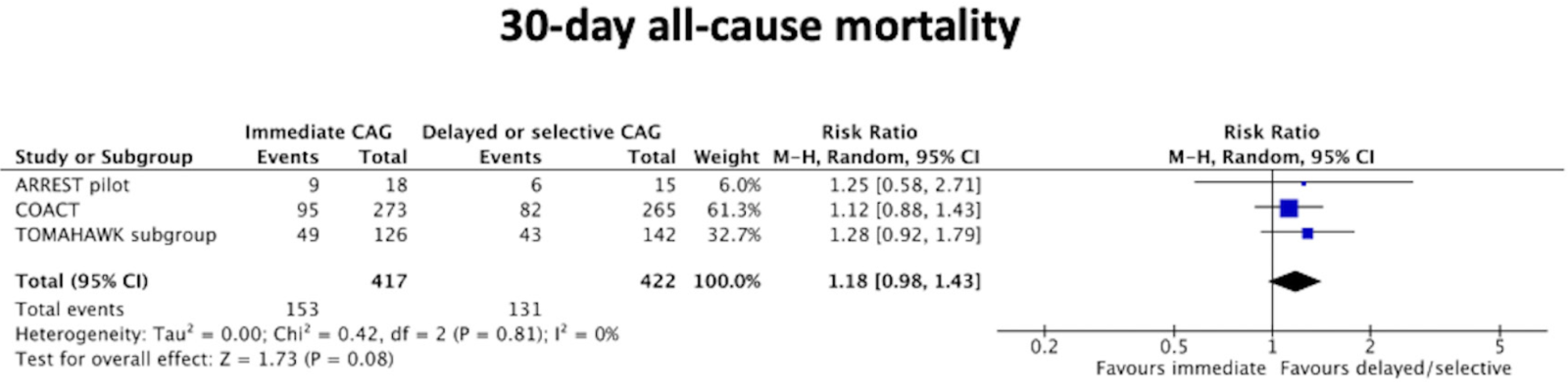
Recent randomized control trials (RCTs) have shown no benefit of early coronary angiography (CAG) in survivors of out-of-hospital cardiac arrest (OHCA) without ST-segment elevation on the electrocardiography (ECG). However, most studies included both those with an initial non-shockable and shockable rhythm. It is well recognized that OHCA patients with non-shockable rhythm have significantly worse outcomes and these patients are less likely to present with coronary artery occlusion than those survivors with shockable rhythm. We aimed to conduct a meta-analysis of RCTs to evaluate the impact of timing of CAG on 30-day all-cause mortality in survivors of OHCA presenting with an initial shockable rhythm and without ST-segment elevation. A comprehensive search of the major databases was conducted and eligible RCTs were identified. The primary endpoint was 30-day all-cause mortality. Risk ratios (RRs) with 95% confidence intervals (CI) were used as summary estimates. The pooled RR was calculated with the random-effects model using the Mantel-Haenszel method. All reported P values are two-sided, with significance set at p < 0.05. Three RCTs met the criteria for inclusion in this meta-analysis. A total of 839 OHCA patients with shockable rhythm were included in the 30-day all-cause mortality analysis. There was numerically higher 30-day all-cause mortality in the immediate CAG group (37%) when compared to the delayed/ selective CAG group (31%), but this was not statistically significant [RR 1.18 (95% CI 0.98-1.43), P=0.08, I2 0%]. Our analysis demonstrates that in patients surviving an OHCA secondary to an initial shockable rhythm, and without ST-segment elevation on ECG, an early CAG strategy was not superior to a delayed or selective CAG strategy. Therefore, an initial delayed or selective strategy can be safely adopted in these patients.
Keywords: Out-of-hospital cardiac arrest, Coronary angiography, Mortality, ST-segment elevation, Shockable rhythm
Abstract
Recent randomized control trials (RCTs) have shown no benefit of early coronary angiography (CAG) in survivors of out-of-hospital cardiac arrest (OHCA) without ST-segment elevation on the electrocardiography (ECG). However, most studies included both those with an initial non-shockable and shockable rhythm. It is well recognized that OHCA patients with non-shockable rhythm have significantly worse outcomes and these patients are less likely to present with coronary artery occlusion than those survivors with shockable rhythm. We aimed to conduct a meta-analysis of RCTs to evaluate the impact of timing of CAG on 30-day all-cause mortality in survivors of OHCA presenting with an initial shockable rhythm and without ST-segment elevation. A comprehensive search of the major databases was conducted and eligible RCTs were identified. The primary endpoint was 30-day all-cause mortality. Risk ratios (RRs) with 95% confidence intervals (CI) were used as summary estimates. The pooled RR was calculated with the random-effects model using the Mantel-Haenszel method. All reported P values are two-sided, with significance set at p < 0.05. Three RCTs met the criteria for inclusion in this meta-analysis. A total of 839 OHCA patients with shockable rhythm were included in the 30-day all-cause mortality analysis. There was numerically higher 30-day all-cause mortality in the immediate CAG group (37%) when compared to the delayed/ selective CAG group (31%), but this was not statistically significant [RR 1.18 (95% CI 0.98-1.43), P=0.08, I2 0%]. Our analysis demonstrates that in patients surviving an OHCA secondary to an initial shockable rhythm, and without ST-segment elevation on ECG, an early CAG strategy was not superior to a delayed or selective CAG strategy. Therefore, an initial delayed or selective strategy can be safely adopted in these patients.
Keywords: Out-of-hospital cardiac arrest, Coronary angiography, Mortality, ST-segment elevation, Shockable rhythm
Introduction
Out-of-hospital cardiac arrest (OHCA) is a leading cause of mortality globally, despite advancements in resuscitative and intensive care management (Myat et al., 2018), with up to 40% of patients dying after successful resuscitation, with an initial shockable rhythm (Patel et al., 2016). The exact cause is often unclear directly after the event, but the presence of ST-segment elevation on post resuscitation electrocardiography (ECG) is a robust predictor of an acute coronary occlusion triggering the cardiac arrest. Despite this, a large proportion of OHCA patients are found to have no ST-segment elevation on their electrocardiography (ECG), making the list of potential cardiac and noncardiac causes considerably larger.
Coronary artery disease is the leading cause of cardiac arrest, with acute coronary occlusion accounting for up to 60% of all OHCA (Geri et al., 2017). Early revascularization in patients with acute coronary occlusion can preserve ventricular function, limit myocardial damage, and reduce the likelihood of life-threatening arrhythmias (Lemkes et al., 2019). However, routine early coronary angiography (CAG) on all patients post OHCA exposes those without acute coronary artery occlusion to unnecessary procedural risk, potential complications, and delays in the identification of the cause of the cardiac arrest and subsequent treatment. Former observational studies looking at early CAG in OHCA patients without ST-segment elevation showed conflicting results (Bro-Jeppesen et al., 2012; Hollenbeck et al., 2014; Dumas et al., 2016; Staudacher et al., 2018). This led the American Heart association (AHA) to recommend that immediate CAG could reasonably be considered for unstable patients, comatose after OHCA without ST elevation but with a high suspicion of cardiac cause (Class IIa; Level of Evidence B-nonrandomised) (O’Connor et al., 2015).
However, several randomized controlled trials (RCTs) have been published in the field over the past few years. Following the publication of the COACT trial (Lemkes et al., 2019) in 2019, the 2020 European Society of Cardiology (ESC) guideline for non-ST-segment elevation myocardial infarction, recommends delayed as opposed to immediate CAG, amongst successfully resuscitated OHCA patients without ST-segment elevation (Class IIa: level of evidence B – single randomised clinical trial) (Collet et al., 2021). Since then, the TOMAHAWK trial (Desch et al., 2021) has recently been published and the latest meta-analysis (Abusnina et al., 2021) of all RCTs published to date showed no mortality benefit with immediate CAG in OHCA patients without ST-segment elevation. Of note, both patients with shockable and non-shockable rhythms were included in most of the RCTs included. It is well recognized that OHCA patients with non-shockable rhythm have significantly worse outcomes (Meaney et al., 2010) and these patients are less likely to present with coronary artery occlusion than those survivors with shockable rhythm (Geri et al., 2017; Wilson et al., 2017). Therefore, grouping both shockable and non-shockable rhythm OHCA survivors together in previous analysis may have diluted the potential benefit of early CAG in those OHCA survivors with shockable rhythm.
Therefore, we aimed to conduct a meta-analysis of all RCTs published to date, to assess the impact of early CAG on 30-day all-cause mortality, in OHCA survivors with an initial shockable rhythm but without ST-segment elevation.
Methods
This study was performed according to the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2011) recommendations.
Eligibility criteria
All RCTs investigating immediate CAG versus delayed/selective CAG in OHCA survivors with an initial shockable rhythm, without ST elevation were eligible for inclusion in the meta-analysis. RCTs comparing non-shockable rhythms or a mixture of shockable and non-shockable rhythms and not reporting outcomes by subgroup were excluded.
Search strategy
We searched PubMed/MEDLINE and Ovid/Embase from inception through to the 20th of March 2022 for studies in English and published as a full-text article. Furthermore, the references of the eligible papers were screened to identify any other potential studies.
Study selection
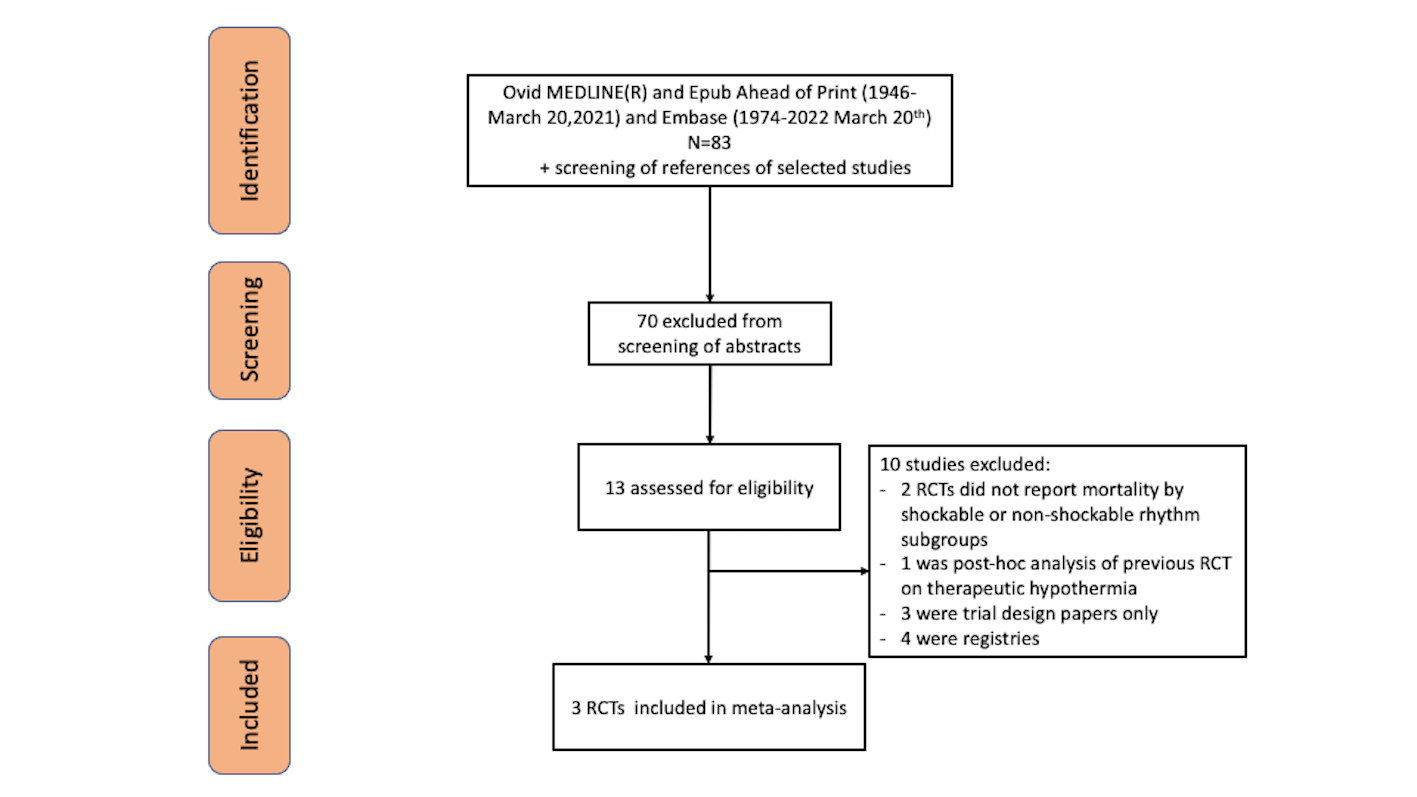
Two authors (BAL, HB) identified suitable articles and their supplemental appendix and extracted the data independently and in duplication. Any disagreements in data extraction were resolved by consensus. Figure 1 shows the process of study selection as per preferred reporting items for systematic reviews and meta-analyses (PRISMA)(Moher et al., 2009).
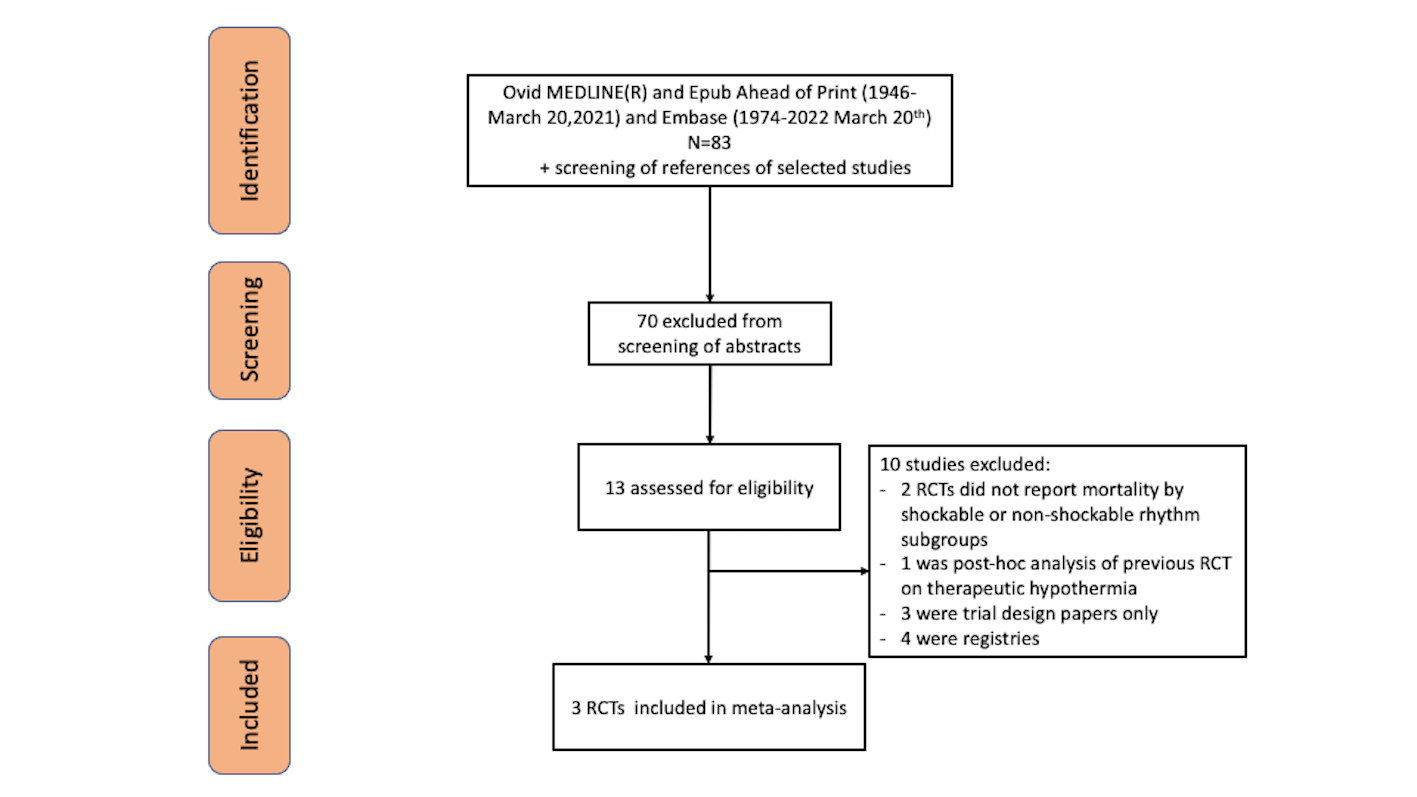
In a new window | Download PPT
Figure 1: PRISMA flow diagram of the search for published trials showing search strategy with excluded studies and reason for exclusion.
Data extraction and quality assessment
Characteristics of the RCTs included, baseline clinical characteristics of the study population, and individual clinical endpoints were extracted. Risk of bias was assessed as recommended by the Cochrane Handbook (Higgins et al., 2011) but without constructing a composite quality score, given the limitations inherent to such an approach (Jüni et al., 1999). We aimed to produce a funnel plot if there were >10 included RCTs in the forest plot to assess for publication bias.
Endpoints
The main endpoint of interest was all-cause mortality at 30 days. Mortality data was extracted at 30 days from Kaplan-Meier curves for RCTs reporting longer duration of follow-up. Event rates were extracted from the intention-to-treat analysis from each trial.
Statistical analysis
Statistical analysis was performed using RevMan 5.4 (Nordic Cochrane Centre). Risk ratios (RRs) with 95% confidence intervals (CI) were used as summary estimates. Heterogeneity among trials was quantified using I2 statistics with I2 of 0-25%, 25-50% and 50-75% considered as low, moderate, and high heterogeneity, respectively. The pooled RR was calculated with the random-effects model using the Mantel-Haenszel method. All reported p values are two-sided, with significance set at p < 0.05. For sensitivity analysis, we tested the robustness of each result by removing one trial at a time.
Results
Selection of RCTs
Figure 1 shows the PRISMA diagram of the search and selection strategy. A total of 83 studies were identified and 13 RCTs were eventually selected for full-text review. After reviewing the references of the shortlisted studies, 3 RCTs met the criteria for inclusion in this meta-analysis.
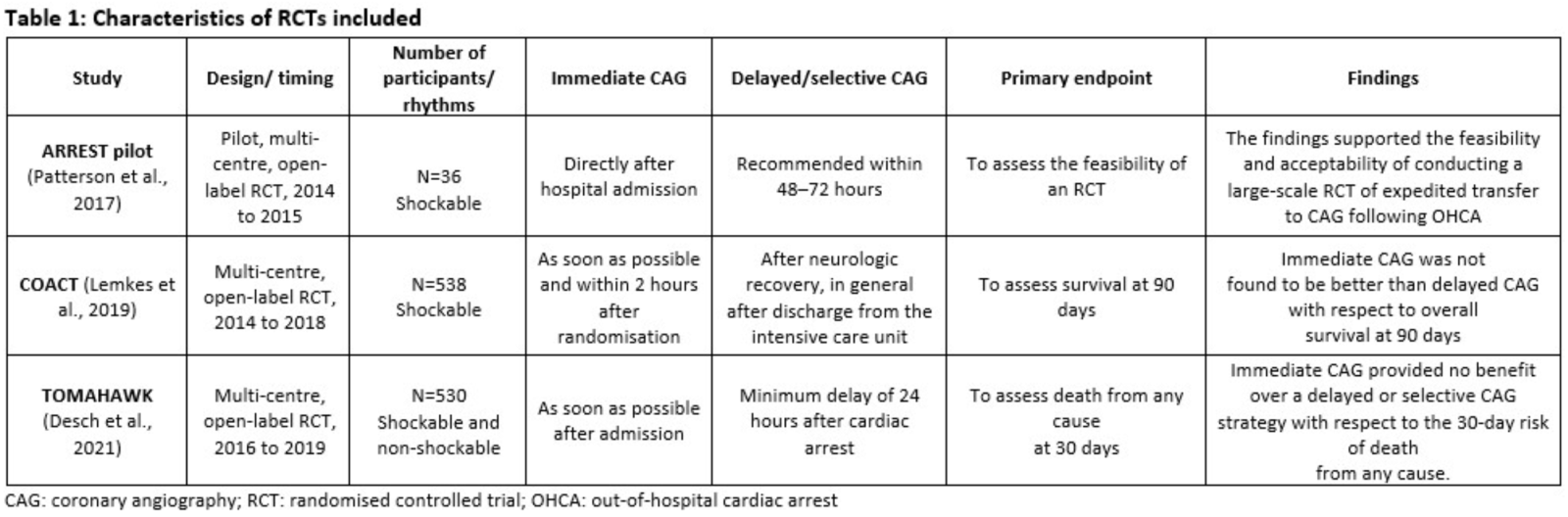
Included studies
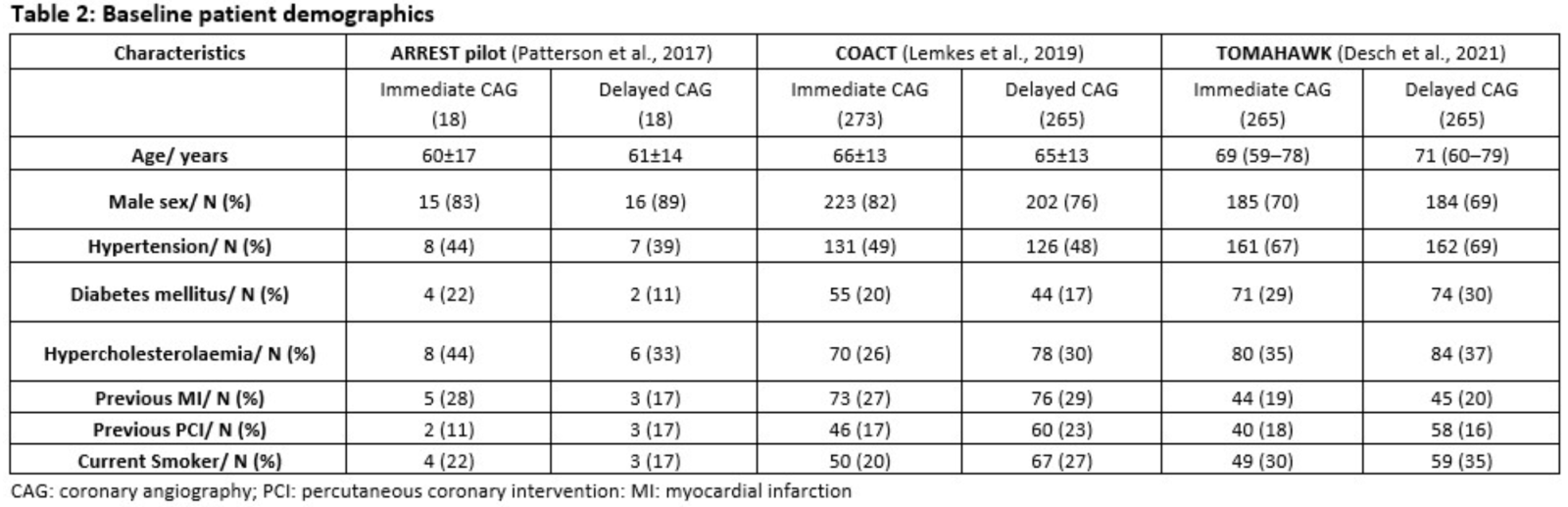
The characteristics of the three RCTs included are provided in Table 1. The ARREST pilot study (Patterson et al., 2017) included 36 OHCA patients with shockable rhythm and 30-day all-cause mortality data was available in 33 patients. The COACT trial (Lemkes et al., 2019) included 538 OHCA patients with shockable rhythm and reported 90-day all-cause mortality. However, 30-day all-cause mortality was available via their Kaplan-Meier curve in their paper (none of the patients were lost to follow-up or censored). The TOMAHAWK trial (Desch et al., 2021) included 530 patients with both shockable and non-shockable rhythm in their study but they also reported 30-day all-cause mortality by those subgroups. Half of their cohort involved patients with shockable rhythm and therefore this subgroup was use for the 30-day all-cause mortality analysis. Table 1 provides the baseline characteristics of the total cohort from the TOMAHAWK trial (Desch et al., 2021).
The patients were in their sixties on average and the majority were male. There was a high prevalence of the conventional risk factors for CAD such as hypertension, diabetes mellitus, hypercholesterolaemia, and smoking history (Table 2).
30-day all-cause mortality
A total of 839 OHCA patients with shockable rhythm were included in the 30-day all-cause mortality analysis. There was numerically higher 30-day all-cause mortality in the immediate CAG group (37%) when compared to the delayed/selective CAG group (31%), but this was not statistically significant [RR 1.18 (95% CI 0.98-1.43), P=0.08, I2 0%] as shown in the Forest plot in Figure 2.
Sensitivity analysis
Sensitivity analysis was performed by removing one study at a time from the analysis and there was no difference in 30-day all-cause mortality when immediate CAG was compared to delayed/selective CAG.
Discussion
This meta-analysis from 3 RCTs, including 839 patients, demonstrates that in patients surviving OHCA with an initial shockable rhythm, and without ST-segment elevation on ECG, early CAG strategy provided no survival benefit at 30 days, but there was a trend towards more deaths, when compared to a delayed/selective CAG strategy.
Our findings are consistent with the COACT trial (Lemkes et al., 2019), which included a total of 552 OHCA patients with an initial shockable rhythm, and also showed no mortality benefit at 90 days with an early CAG strategy. Our analysis also included the subgroup with shockable rhythm from the TOMAHAWK trial (Desch et al., 2021) and the ARREST pilot study (Patterson et al., 2017). Our analysis strengthens the current evidence that even in survivors of OHCA presenting with an initial shockable rhythm and hemodynamically stable, a delayed or selective CAG strategy should be adopted. We did find a trend towards more deaths in the immediate CAG arm. Of note, an acute unstable lesion or thrombotic lesion was present in only 17% of patients in the COACT trial (Lemkes et al., 2019). Given that the predominant cause of death was from hypoxic brain injury as shown in the COACT trial (Lemkes et al., 2019), it may be plausible that immediate CAG in those with a lower probability of having obstructive coronary lesions than those presenting with an ST-segment elevation myocardial infarction, leads to a delay in other therapeutic interventions, such as therapeutic cooling for cerebral protection. Our findings also build upon the recent metanalysis by Abusnina et al., 2021, which included studies of OHCA patients with both shockable and non-shockable rhythms and showed no benefit of an early CAG strategy when compared to the delayed/selective CAG strategy.
The 2017 ESG guideline for STEMI (Ibanez et al., 2018) does recommend urgent CAG in patients with resuscitated cardiac arrest without diagnostic ST segment elevation but with a high suspicion of ongoing myocardial ischemia (class of recommendation IIa; level of evidence C), but this recommendation pre-dates the publication of the landmark COACT trial (Lemkes et al., 2019). Although the 2020 ESC guideline for non-ST-segment elevation myocardial infarction (Collet et al., 2021) has subsequently recommended a delayed as opposed to an immediate CAG strategy in these patients, the class of recommendation was IIa with a level of evidence B as this was based on the COACT trial (Lemkes et al., 2019) alone. However, following the recently published RCTs and meta-analysis in the field (Abusnina et al., 2021), including the result of our work, we would anticipate the next ESC guideline for STEMI and NSTEMI to strengthen their recommendation to class I, with a level of evidence A to delay CAG as opposed to immediate CAG, for successfully resuscitated OHCA patients without ST-segment elevation and without hemodynamically stability.
Our meta-analysis has several strengths. Pooling data from three RCTs provided more statistical power to support our findings as highlighted by the narrow 95% confidence interval for 30-day all-cause mortality. Two of the three RCTs were multi-national trials, which increases the generalizability. However, our study is not without limitations. This was a study-level meta-analysis rather than a patient-level meta-analysis and therefore we excluded studies that reported OHCA patients with any initial rhythm disturbance as a combined group. Furthermore, as a result, we could not assess the subgroup with non-shockable rhythm separately. Furthermore, we only analyzed 30-day mortality and we did not have data on secondary endpoints such as survival rate with no or minimal residual neurological sequelae. The DISCO (NCT02309151), COUPE (NCT02641626), and ARREST (NCT03872960) trials investigating the role of immediate versus delayed/selective CAG in OHCA survivors are currently ongoing and their results are eagerly awaited. Future patient-level meta-analysis of RCTs with longer duration of follow-up and secondary parameters such as cerebral performance category will provide further valuable insights in this group of patients.
Conclusions
Our meta-analysis of RCTs in patients with OHCA due to an initial shockable rhythm, without ST-segment elevation on ECG, found that immediate CAG did not provide a mortality benefit at 30-days and therefore an initial delayed or selective strategy can be safely adopted in these patients. Future guidelines should be able to provide a stronger level of recommendations to guide clinicians on timing of CAG in this group of patients.
Competing interests
None of the authors have any competing interests related to this work.
Funding
None
Acknowledgements
None
References
Bethany Alice Lane1,2
1Imperial College, London, UK. 2St. Bartholomew's Hospital, London, UK.
Heerajnarain Bulluck*3,4
3Yorkshire Heart Centre, Leeds General Infirmary, Leeds Teaching Hospitals NHS Trust, Leeds, UK. 4Leeds Institute of Cardiovascular and Metabolic Medicine, University of Leeds, Leeds, UK
Corresponding author:
Dr Heerajnarain Bulluck, PhD
Email: h.bulluck@leeds.ac.uk
In a new window | Download PPT
Figure 1: PRISMA flow diagram of the search for published trials showing search strategy with excluded studies and reason for exclusion.
Supporting Information
Metrics
| Full-Text | Supporting Information | ||
|---|---|---|---|
| Number | 7696 | 6 | 0 |
Copyright © 2017 Conditioning Medicine, All Rights Reserved.
Address: Conditioning Medicine Editorial Office, 3500 Terrace Street, Pittsburgh, PA, 15213, USA